Shingles and diabetes are two common but serious health conditions. When they occur together, managing them becomes even more critical. Shingles, caused by the reactivation of the varicella-zoster virus, often leads to painful rashes and nerve pain. On the other hand, diabetes weakens the immune system, making individuals more susceptible to infections like shingles. Therefore, understanding how these conditions interact and learning how to manage them is essential for anyone affected.
In this guide, we’ll explore the link between shingles and diabetes, outline symptoms, discuss prevention strategies, and provide effective treatment options — including the use of Pregabalin 300 mg for nerve pain relief.
Understanding Shingles
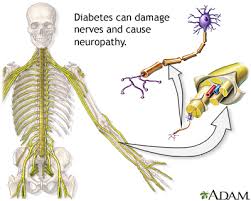
Shingles, also known as herpes zoster, is a viral infection that affects the nerves. It occurs when the varicella-zoster virus (which causes chickenpox) reactivates later in life. This reactivation is more likely in people with weakened immune systems, such as those with diabetes.
Common Symptoms of Shingles
-
Painful, blistering skin rash (typically on one side of the body)
-
Burning, tingling, or itching sensation
-
Fever and chills
-
Headache
-
Fatigue
-
Sensitivity to touch or light
While the rash itself may disappear within weeks, nerve pain—called postherpetic neuralgia (PHN)—can persist for months or even years.
How Diabetes Increases Shingles Risk
Diabetes impairs immune function. As a result, individuals with diabetes have a higher risk of developing infections, including shingles. High blood sugar levels make it harder for the body to fight off viruses and recover from them.
Moreover, people with diabetes are more prone to complications once shingles sets in. These complications may include:
-
Longer healing time
-
Greater risk of nerve damage
-
Higher chances of postherpetic neuralgia
-
Elevated blood glucose levels due to stress or infection
Because of these risks, early diagnosis and effective treatment become especially important.
Diagnosis and Early Intervention
When someone with diabetes shows symptoms of shingles, a healthcare provider may perform the following:
-
Clinical examination of the rash
-
Lab tests (e.g., PCR tests for varicella-zoster DNA)
-
Blood sugar testing to check for imbalances
Early intervention significantly reduces the severity and duration of shingles. Doctors typically recommend antiviral drugs within 72 hours of rash onset to limit virus replication.
Treatment Options for Shingles in Diabetics
People with both shingles and diabetes require a tailored treatment plan. The goal is to manage the infection, reduce pain, prevent complications, and control blood sugar levels simultaneously.
Here are the primary treatment options:
1. Antiviral Medications
Doctors commonly prescribe antivirals such as acyclovir, valacyclovir, or famciclovir. These drugs help stop the virus from multiplying, thereby reducing the duration and severity of symptoms.
2. Pain Management with Neuropathic Agents
Pain is the most debilitating symptom of shingles, especially in diabetic patients who are already prone to neuropathy. That’s where nerve pain medications come in.
Pregabalin 300 mg is one of the most effective treatments for nerve pain caused by shingles. It belongs to a class of drugs known as anticonvulsants and works by calming overactive nerves.
Benefits of using Pregabalin 300 mg include:
-
Significant relief from nerve pain
-
Improved sleep quality
-
Reduced anxiety, often associated with chronic pain
-
Fewer side effects compared to traditional painkillers
Doctors usually start with a lower dose and gradually increase it to Pregabalin 300 mg, depending on the patient’s condition and tolerance level.
3. Blood Sugar Management
Infection and stress can spike blood glucose levels. Therefore, it’s essential to monitor and manage blood sugar diligently during a shingles episode. Adjusting insulin or oral hypoglycemics may be necessary under medical supervision.
4. Topical Treatments
Lidocaine patches or creams can help numb the affected area. These are often used in combination with oral medications like Pregabalin 300 mg for enhanced pain control.
5. Anti-inflammatory Drugs
Over-the-counter NSAIDs like ibuprofen may help reduce inflammation and discomfort, but they must be used cautiously in diabetics due to kidney concerns.
Preventing Shingles in Diabetics
Prevention remains the best strategy. The CDC recommends the shingles vaccine (Shingrix) for adults over 50, including those with chronic conditions like diabetes. The vaccine is over 90% effective at preventing shingles and postherpetic neuralgia.
Other preventive measures include:
-
Keeping blood sugar levels in check
-
Practicing good hygiene
-
Avoiding contact with individuals who have active shingles
-
Managing stress to avoid immune suppression
Postherpetic Neuralgia (PHN) and Diabetes
PHN is a lingering nerve pain that can occur after the shingles rash heals. Diabetic individuals are more likely to develop PHN due to existing nerve sensitivity.
Common symptoms of PHN include:
-
Sharp, shooting pain
-
Sensitivity to light touch
-
Constant burning or aching in the affected area
Pregabalin 300 mg is the first-line treatment for PHN. Studies show that patients using Pregabalin 300 mg report reduced pain intensity and improved daily functioning. It also helps restore quality sleep, which is often disturbed due to nighttime pain.
In some cases, doctors may also recommend antidepressants like amitriptyline or duloxetine for additional pain relief.
Coping Strategies for Patients
Managing shingles with diabetes isn’t only about medication. Patients must adopt a holistic approach for better outcomes. Here are some helpful strategies:
1. Stay Hydrated and Eat Balanced Meals
Proper nutrition supports immune function and helps maintain stable blood sugar levels. Include antioxidant-rich foods to speed up recovery.
2. Get Plenty of Rest
Rest is essential for healing. It helps the body recover from both the infection and the stress it places on the immune system.
3. Apply Cool Compresses
Cool, damp cloths on the rash can relieve itching and burning sensations.
4. Avoid Scratching
Scratching can lead to secondary infections, especially dangerous for diabetics. Keep nails trimmed and consider wearing gloves at night.
When to Seek Immediate Medical Help
While shingles can often be treated at home, certain situations demand urgent medical attention:
-
Rash spreads to the eyes or face
-
Severe, unrelenting pain despite using Pregabalin 300 mg
-
Signs of infection such as pus, fever, or increasing redness
-
High or unstable blood sugar levels
-
Confusion or dizziness
Prompt medical care can prevent complications and reduce long-term impact.
Conclusion
Shingles and diabetes form a dangerous duo that demands immediate and comprehensive attention. From antiviral drugs and blood sugar monitoring to effective nerve pain management with Pregabalin 300 mg, each component plays a vital role in the healing journey. Fortunately, early intervention and consistent care can minimize discomfort and prevent lasting damage.
By understanding the connection between these two conditions and acting quickly, patients can improve outcomes and lead a better quality of life. Always consult your healthcare provider for the best treatment plan tailored to your needs.