No Scalpel Vasectomy has become one of the most advanced and refined procedures in modern urology. Designed to provide permanent male contraception with minimal invasiveness, this technique replaces traditional incisions with a small puncture approach that reduces trauma, bleeding, and recovery time. As surgical technologies evolve, No Scalpel Vasectomy now benefits from enhanced visualization tools, precision instruments, and refined procedural protocols that improve outcomes and patient comfort.
Modern surgical precision is not only about advanced equipment—it also reflects improved training, data-driven decision-making, and standardized techniques that minimize risks. Today’s urologists rely on a combination of experience, evidence-based practices, and innovative tools to deliver safer and more efficient procedures. This article explores how modern surgical precision has transformed No Scalpel Vasectomy, highlighting technological innovations, clinical strategies, patient outcomes, and the future of this minimally invasive method.
Understanding the No Scalpel Vasectomy Technique
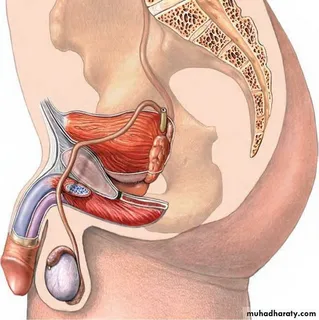
No Scalpel Vasectomy differs significantly from traditional vasectomy methods. Instead of making one or two incisions with a scalpel, the surgeon uses a specialized instrument to create a tiny puncture in the scrotal skin. Through this opening, the vas deferens—the tubes that carry sperm—are gently isolated, sealed, or divided.
This approach minimizes tissue disruption and reduces surgical trauma. The absence of large incisions means fewer sutures, less bleeding, and a faster recovery period. The technique has been refined over decades and is now considered a gold standard in many countries.
Modern surgical precision enhances this process through careful preoperative planning and standardized procedural steps. Surgeons are trained to identify anatomical structures accurately and perform delicate manipulations that reduce complications such as hematomas or infections. As a result, patients experience shorter procedures and improved comfort during and after surgery.
The Role of Advanced Surgical Instruments
Modern surgical precision in No Scalpel Vasectomy heavily relies on specialized instruments designed for minimal invasiveness. Tools such as ring clamps and sharp-tipped dissectors allow surgeons to stabilize and access the vas deferens without large incisions. These instruments enable precise movements and controlled tissue handling.
High-quality surgical materials also contribute to improved outcomes. Advanced sealing methods, including cauterization or fascial interposition, are performed with precision to prevent sperm leakage and reduce the risk of failure. The use of refined instruments ensures consistent results and helps surgeons maintain accuracy even in complex anatomical situations.
Furthermore, improvements in sterilization protocols and instrument ergonomics enhance procedural safety and efficiency. Modern surgical sets are designed to reduce hand fatigue and allow surgeons to maintain steady control during delicate steps, which is essential for maintaining precision.
Enhanced Visualization and Imaging Techniques
One of the most significant advancements in No Scalpel Vasectomy is the integration of enhanced visualization technologies. Although the procedure is relatively straightforward, modern surgical precision benefits from magnification tools and improved lighting systems that allow surgeons to identify structures more clearly.
Some clinics utilize ultrasound or advanced imaging during complex cases to map anatomical variations before surgery. These technologies help surgeons anticipate challenges and adjust their techniques accordingly. Even minor improvements in visualization can reduce accidental damage to surrounding tissues and improve procedural accuracy.
In addition, digital record systems and surgical analytics help practitioners evaluate outcomes and refine their approaches over time. By analyzing data from previous procedures, surgeons can identify patterns and optimize techniques to achieve consistent results.
Precision-Based Anesthesia Approaches
Local anesthesia is a cornerstone of No Scalpel Vasectomy, and modern precision extends to anesthetic administration as well. Advanced injection techniques allow surgeons to deliver anesthesia accurately while minimizing discomfort. Methods such as no-needle jet injectors or buffered anesthetic solutions have improved patient experience during the procedure.
Precise anesthesia placement ensures that patients remain comfortable without excessive medication use. This targeted approach reduces side effects and allows for faster recovery after the procedure. By combining modern anesthesia techniques with minimally invasive surgical methods, clinicians achieve a smoother overall experience for patients.
Standardized Protocols and Training
Modern surgical precision is not solely dependent on technology—it also relies on rigorous training and standardized protocols. Urologists undergo specialized education to master the No Scalpel Vasectomy technique, focusing on anatomical knowledge, patient communication, and complication prevention.
Simulation-based training has become increasingly common, allowing surgeons to practice precision skills in controlled environments before performing real procedures. Continuous medical education ensures that practitioners stay updated on evolving best practices and technological advancements.
Standardization of procedural steps contributes to consistency across different clinics. Clear guidelines on patient selection, sterilization methods, and post-procedure care reduce variability and enhance overall safety. These protocols ensure that patients receive high-quality care regardless of where the procedure is performed.
Reduced Complications Through Precision
One of the most significant benefits of modern surgical precision in No Scalpel Vasectomy is the reduction in complications. The minimally invasive nature of the technique already lowers the risk of infection and bleeding compared to traditional methods. However, precision-based approaches further enhance safety.
Accurate identification of the vas deferens prevents accidental injury to surrounding structures. Controlled cauterization and sealing techniques minimize the risk of recanalization, where the vas deferens reconnects. Precise handling of tissues also reduces postoperative swelling and discomfort.
Modern follow-up protocols allow clinicians to monitor patients closely and address any concerns early. Telehealth consultations and digital symptom tracking provide convenient ways for patients to communicate with healthcare providers, ensuring timely intervention if complications arise.
Patient-Centered Outcomes and Satisfaction
Modern surgical precision not only improves clinical outcomes but also enhances patient satisfaction. Many individuals choose No Scalpel Vasectomy because it offers shorter recovery times and less postoperative discomfort. Precision-driven methods further support these benefits by minimizing tissue trauma and ensuring consistent results.
Patients often report confidence in procedures performed with advanced techniques and modern technology. Clear communication, precise anesthesia administration, and efficient surgical processes contribute to a positive overall experience. Additionally, improved counseling tools help patients understand what to expect, reducing anxiety before and after surgery.
High satisfaction rates are also linked to the procedure’s effectiveness. When performed with precision, No Scalpel Vasectomy has a very low failure rate, reinforcing trust in the technique as a reliable form of permanent contraception.
Integration of Digital Health and Data Analytics
Digital health technologies are becoming an integral part of modern surgical precision. Electronic health records allow surgeons to track patient histories, allergies, and prior procedures with accuracy. Data analytics help identify trends and optimize patient selection criteria.
Some clinics use digital platforms for preoperative education, ensuring patients receive consistent information about preparation and recovery. Postoperative monitoring apps enable patients to report symptoms and receive guidance without unnecessary clinic visits.
Artificial intelligence is also emerging as a tool for predicting complication risks and assisting in clinical decision-making. Although still in early stages, AI-driven analytics may soon help surgeons personalize procedural strategies based on individual patient characteristics.
Future Innovations in Surgical Precision
The future of No Scalpel Vasectomy and modern surgical precision is promising. Advancements in robotic-assisted micro-instrumentation and real-time imaging could further refine procedural accuracy. New materials for sealing the vas deferens may enhance long-term reliability and reduce complications even further.
Research into regenerative medicine and improved pain management techniques may also influence postoperative recovery. As medical education continues to evolve, surgeons will gain access to more sophisticated training tools that enhance precision and confidence.
Global collaboration among urologists and researchers is expected to drive innovation and standardize best practices worldwide. These developments will likely make No Scalpel Vasectomy even safer, more efficient, and more accessible to patients seeking permanent contraception.
Conclusion
No Scalpel Vasectomy represents a significant advancement in male reproductive healthcare, and modern surgical precision has elevated its effectiveness and safety. Through specialized instruments, enhanced visualization, precision-based anesthesia, and standardized training, today’s procedures achieve remarkable outcomes with minimal invasiveness.
The integration of digital health technologies and data-driven decision-making further supports consistent results and improved patient satisfaction. As new innovations continue to emerge, No Scalpel Vasectomy will remain at the forefront of minimally invasive surgery, offering individuals a reliable and comfortable option for permanent contraception.
Modern surgical precision is not just a technical concept—it is a holistic approach that combines technology, expertise, and patient-centered care. With ongoing advancements and continued commitment to excellence, the future of No Scalpel Vasectomy promises even greater improvements in safety, efficiency, and overall patient experience.
FAQs
1. What makes No Scalpel Vasectomy more precise than traditional vasectomy?
No Scalpel Vasectomy uses specialized instruments and a puncture technique instead of large incisions. Modern surgical precision includes improved visualization, refined anesthesia methods, and standardized protocols that enhance accuracy and reduce complications.
2. Does modern surgical precision reduce recovery time after No Scalpel Vasectomy?
Yes. Precision-based techniques minimize tissue damage and bleeding, leading to faster healing and less postoperative discomfort. Most patients can return to normal activities within a few days, depending on medical advice.
3. Is No Scalpel Vasectomy with modern surgical precision considered safe?
When performed by trained professionals, it is considered a safe and highly effective procedure. Advances in technology, training, and data-driven practices have significantly reduced complication rates and improved overall outcomes.