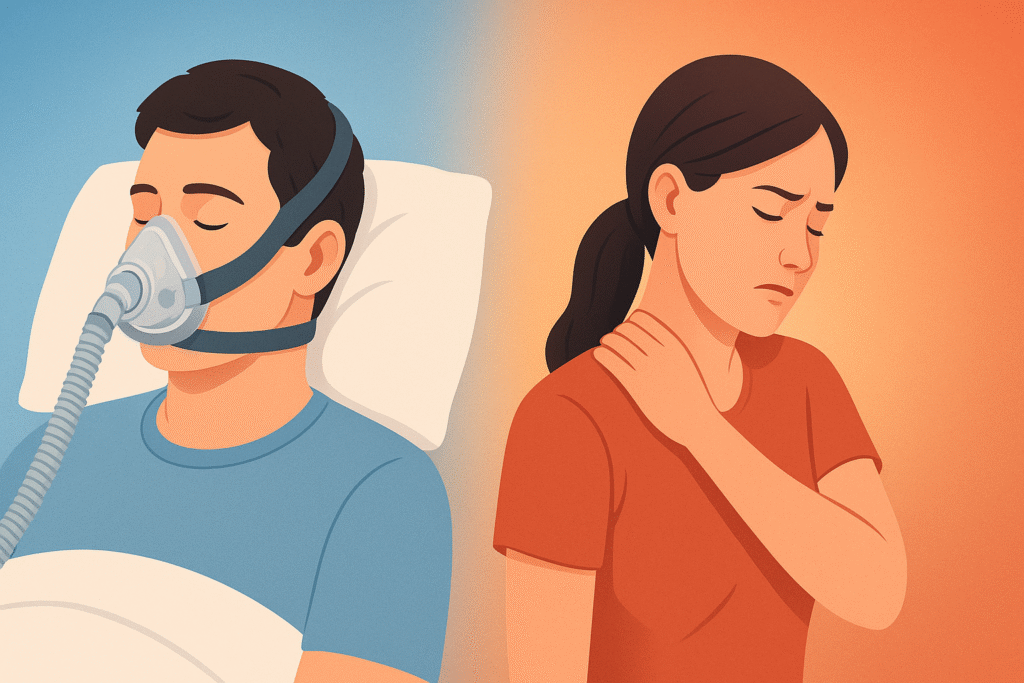
The sleep apnea and chronic pain link is an area of growing interest among medical researchers and clinicians. While sleep apnea is often associated with loud snoring and daytime fatigue, its effects reach far beyond poor rest. Emerging evidence shows that untreated sleep apnea can worsen chronic pain conditions, while chronic pain itself may interfere with sleep, creating a difficult cycle that affects overall health and well-being. Understanding how these two conditions interact is essential for finding effective treatment strategies.
Understanding Sleep Apnea
Sleep apnea is a disorder in which breathing repeatedly stops and starts during sleep. The most common type, obstructive sleep apnea (OSA), happens when throat muscles relax too much, narrowing or blocking the airway.
Common symptoms of sleep apnea include:
- Loud, frequent snoring
- Waking up choking or gasping for air
- Morning headaches
- Excessive daytime sleepiness
- Irritability, poor focus, or memory problems
Untreated sleep apnea raises the risk of serious health issues such as high blood pressure, stroke, heart disease, and type 2 diabetes. It also affects the quality and depth of sleep, which plays a crucial role in how the body perceives and processes pain.
Chronic Pain Explained
Chronic pain is defined as pain that lasts for three months or longer, often persisting beyond the normal healing time. It can be constant or intermittent and is commonly associated with conditions such as:
- Arthritis
- Fibromyalgia
- Back and neck pain
- Migraines
- Neuropathy (nerve pain)
Chronic pain doesn’t just cause physical discomfort—it also impacts emotional well-being, sleep quality, and day-to-day functioning. Poor sleep from pain can lead to greater sensitivity to pain, which further disrupts rest, creating a vicious cycle.
How Sleep and Pain Are Connected
Sleep and pain share a bidirectional relationship. Poor sleep can intensify pain perception, while pain makes it harder to fall and stay asleep. This means:
- Less restorative sleep → more inflammation and heightened sensitivity to pain.
- More pain → fragmented sleep and frequent awakenings.
The cycle feeds itself, and when sleep apnea is added into the mix, the effects become even more complicated and severe.
The Sleep Apnea and Chronic Pain Link
Research suggests that people with sleep apnea are more likely to experience chronic pain conditions, and vice versa. Several mechanisms explain this link:
1. Oxygen Deprivation and Inflammation
During apnea episodes, blood oxygen levels drop. Repeated oxygen deprivation triggers systemic inflammation, which is a known contributor to chronic pain. Conditions like arthritis, fibromyalgia, and migraines may flare or worsen due to increased inflammatory responses.
2. Disrupted Sleep Architecture
Deep sleep stages, particularly slow-wave sleep, play a role in pain modulation and healing. Sleep apnea repeatedly interrupts these stages, leaving the body less equipped to repair tissues and regulate pain sensitivity.
3. Nervous System Overactivation
Apnea episodes cause surges of stress hormones like cortisol and adrenaline. This constant “fight or flight” state sensitizes nerves and heightens pain perception.
4. Opioid Sensitivity
Many people with chronic pain are prescribed opioids. Studies suggest that sleep apnea increases sensitivity to opioids, raising the risk of respiratory depression and worsening apnea severity. This creates a dangerous feedback loop where pain management medications exacerbate sleep issues.
5. Shared Risk Factors
Obesity, sedentary lifestyle, and depression are common risk factors for both sleep apnea and chronic pain. Addressing these underlying factors can improve outcomes for both conditions.
Conditions Where the Link Is Strongest
Fibromyalgia
Fibromyalgia patients often report nonrestorative sleep and widespread pain. Studies show higher rates of undiagnosed sleep apnea in this group. Treating apnea can reduce pain intensity and improve quality of life.
Migraines
Sleep apnea is linked to more frequent and severe migraines. Poor sleep and oxygen fluctuations during the night may act as migraine triggers.
Arthritis
Joint pain worsens when sleep is disrupted. Sleep apnea-related inflammation can compound arthritis pain, making management more difficult.
Chronic Back and Neck Pain
Patients with persistent spinal pain often struggle with insomnia or apnea. Treating sleep disorders can help reduce perceived pain levels.
Impact on Quality of Life
The combined effects of sleep apnea and chronic pain can be devastating:
- Daytime fatigue worsens when both conditions are present, making it harder to maintain work, social, and family responsibilities.
- Mood disorders like anxiety and depression are more likely to develop.
- Reduced physical activity due to pain and fatigue can lead to weight gain, further increasing apnea severity.
- Lower treatment effectiveness for both pain and sleep apnea occurs when one condition is ignored.
This overlap underscores the importance of addressing both conditions in a coordinated way.
Read More: https://pencraftednews.com/
Treatment Approaches
CPAP Therapy
Continuous Positive Airway Pressure (CPAP) is the most common treatment for moderate to severe sleep apnea. It keeps the airway open by delivering pressurized air through a mask. For patients with chronic pain, CPAP can restore restorative sleep and reduce inflammation, which may lower pain intensity over time.
Oral Appliance Therapy
For those who cannot tolerate CPAP, custom oral appliances may help. These devices reposition the jaw and tongue to keep the airway open. They are particularly effective for mild to moderate sleep apnea and can be easier to integrate into daily life.
Lifestyle Interventions
Lifestyle changes benefit both conditions:
- Weight management reduces apnea severity and lowers stress on joints.
- Exercise improves sleep quality, enhances pain tolerance, and reduces inflammation.
- Limiting alcohol and sedatives helps keep airways open and reduces nighttime pain sensitivity.
Pain Management with Sleep in Mind
Doctors treating chronic pain should evaluate patients for possible sleep apnea. Adjusting pain management strategies, especially opioid prescriptions, can reduce risks and improve sleep quality.
Cognitive Behavioral Therapy (CBT)
CBT for insomnia and chronic pain can help patients develop healthier sleep routines, reduce anxiety about pain, and cope more effectively with daily challenges.
Integrated Care Models
The best outcomes come from collaboration between sleep specialists, pain management doctors, and dentists trained in sleep medicine. Addressing both conditions together prevents patients from getting caught in a cycle of untreated pain and poor sleep.
Emerging Research and Innovations
Scientists are exploring new ways to better understand and manage the sleep apnea–chronic pain connection. Some promising areas include:
- Targeted anti-inflammatory therapies aimed at reducing pain caused by sleep-related oxygen deprivation.
- Wearable sleep trackers that detect apnea and monitor pain-related sleep disruptions.
- Neuromodulation therapies to address both sleep disorders and pain sensitivity at the nervous system level.
- Personalized medicine approaches that use genetic, lifestyle, and health data to tailor treatment plans.
As research progresses, patients may gain access to more precise and effective treatment strategies.
Why Awareness Matter
Too often, sleep apnea and chronic pain are treated in isolation. A patient may see a sleep specialist for snoring and fatigue, while another doctor treats their arthritis or migraines. Without recognizing the connection, treatments may be less effective, leaving patients frustrated.
Raising awareness about the sleep apnea and chronic pain link empowers patients to seek comprehensive care. It also encourages healthcare providers to ask the right questions and screen for overlapping conditions.
Final Thoughts
Sleep apnea and chronic pain don’t just coexist—they amplify each other. Poor sleep worsens pain sensitivity, while chronic pain disrupts sleep, creating a cycle that harms health, mood, and daily functioning. Fortunately, effective treatment is available. With the right combination of sleep therapies, pain management, and lifestyle strategies, patients can break the cycle and regain control over their lives. For individuals looking for specialized, holistic care that addresses both conditions together, there are dedicated providers offering Personalized Sleep Apnea Care.